
CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES ›› 2020, Vol. 38 ›› Issue (6): 688-694.doi: 10.12140/j.issn.1000-7423.2020.06.003
• ORIGINAL ARTICLES • Previous Articles Next Articles
ZHU Ji-hai1( ), CAO De-ping2, QIE Yangrangzhong2, LIU Jun2, ZHAO Jun2, LIU Yan2,*(
), CAO De-ping2, QIE Yangrangzhong2, LIU Jun2, ZHAO Jun2, LIU Yan2,*( )
)
Received:2020-07-27
Online:2020-12-30
Published:2021-01-12
Contact:
LIU Yan
E-mail:zhujihai@126.com;543394169@qq.com
Supported by:CLC Number:
ZHU Ji-hai, CAO De-ping, QIE Yangrangzhong, LIU Jun, ZHAO Jun, LIU Yan. Effect of Elsholtzia eriostachya in combination with albendazole in treatment of secondary Echinococcus multilocularis metacestode infection in rats[J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2020, 38(6): 688-694.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.jsczz.cn/EN/10.12140/j.issn.1000-7423.2020.06.003
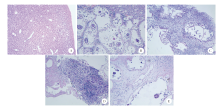
Fig. 1
Histopathological sections of the livers of SD rats after drug treatment (HE staining, ×10) A: Healthy control group showed no evidence of histopathological change in the liver tissue; B: In the infected control group, the cystic cavity and scolex of a typical multifarious echinococcidial larva were seen; C: In the ABZ group, the cystic cavity of the lesion collapsed and the original scolex was rare; D: In the Eriostachys elsholtzia group, there was widespread tissue necrosis and massive infiltration of lymphocytes; E: In the combined treatment group, the focal tissues showed obvious necrosis and hyaline degeneration
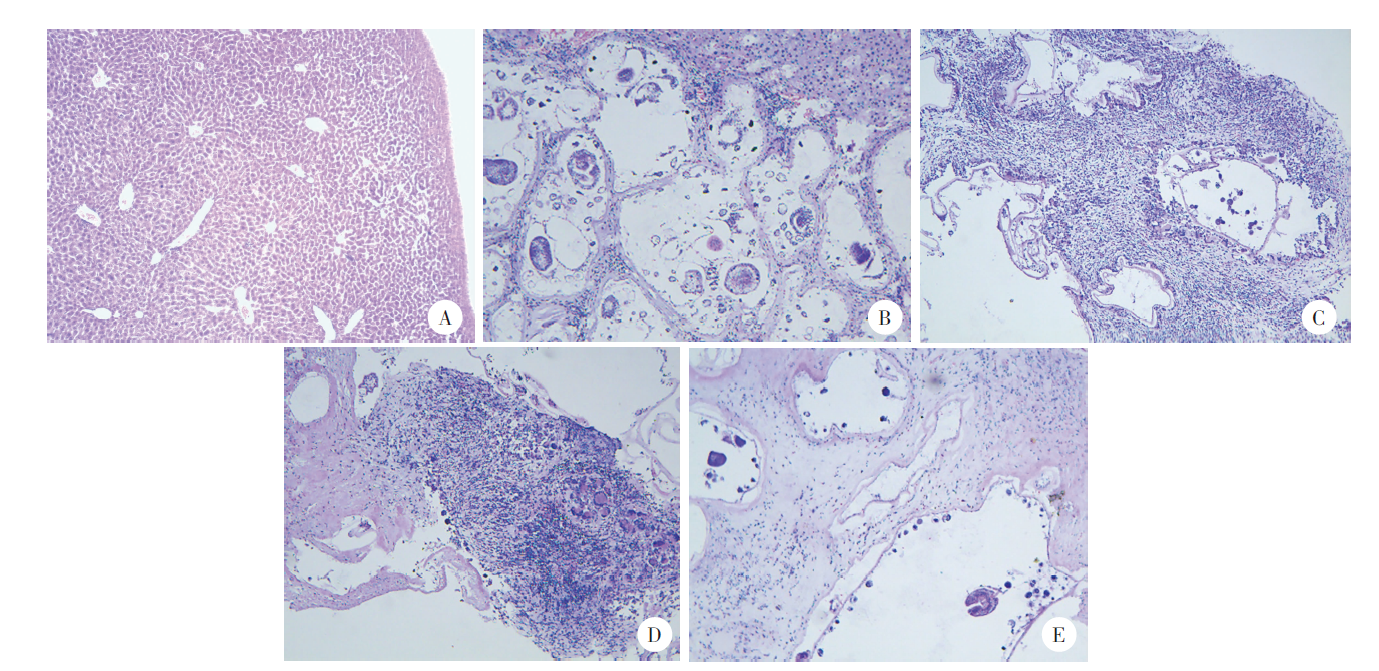

Fig. 2
Histopathological sections of the spleen tissues of SD rats in each group after drug treatment (HE, ×10) A: Healthy control group showed normal morphology of spleen; B: In the infected control group the white pulp region presented a proliferative state; C: In the ABZ group, the white pulp region showed proliferation and irregular morphology; D: In the Eriostachys elsholtzia group, the proliferation of white pulp was evident and a large number of cells which had heteromorphic giant nucleus were observed; E: In the combined treatment group, there was widespread proliferation of large cells, with the loss of red/white pulp differentiation

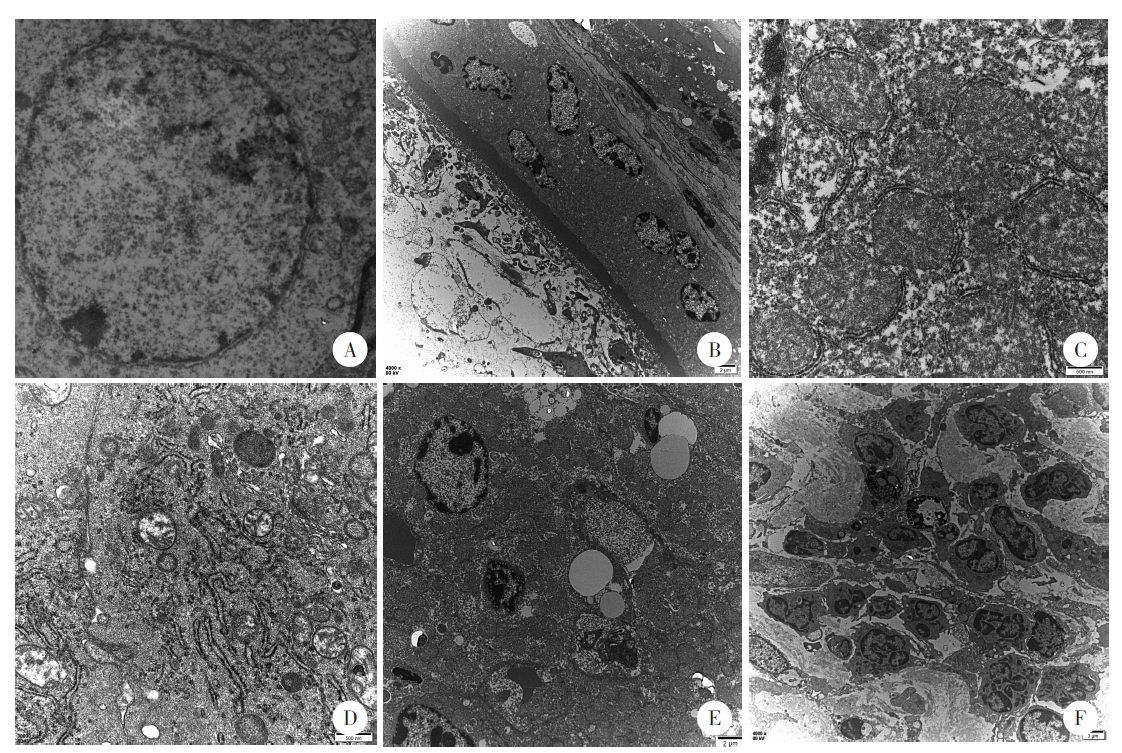
Fig. 3
Transmission electron microscopy (TEM) observation of the ultrastructure of SD rat liver in each group after drug treatment A: The healthy control group showed normal ultrastructure of rat liver (× 4 000); B, C: In the infected control group, there was mitochondrial swelling and the presence of cystic wall-encapsulated hepatocysts (B: × 4 000; C: × 30 000); D: In the combined treatment group, the mitochondria showed vacuolar necrotic (× 30 000); E: In the ABZ group, the cells were irregular in shape with nuclear chromatin condensation (× 4 000); F: In the Eriostachys elsholtzia group, there were significant increases in eosinophils and macrophages in the visual field (× 30 000)
| [1] |
Cadavid Restrepo AM, Yang YR, McManus DP, et al. The landscape epidemiology of echinococcoses[J]. Infect Dis Poverty, 2016,5:13.
pmid: 26895758 |
| [2] |
Deplazes P, Rinaldi L, Alvarez Rojas CA, et al. Global distribution of alveolar and cystic echinococcosis[J]. Adv Parasitol, 2017,95:315-493.
doi: 10.1016/bs.apar.2016.11.001 pmid: 28131365 |
| [3] | Romig T, Deplazes P, Jenkins D, et al. Ecology and life cycle patterns of Echinococcus species[M] //Thompson A. Echinococcus and Echinococcosis, Part A. Amsterdam: Elsevier, 2017: 213-314. |
| [4] | Pensel PE, Castro S, Allemandi D, et al. Enhanced chemoprophylactic and clinical efficacy of albendazole formulated as solid dispersions in experimental cystic echinococcosis[J]. Vet Parasitol, 2014,203(1/2):80-86. |
| [5] | Gao HJ, Chen B, Zhang HB, et al. Pharmacokinetics and liver targeting of lyophilized albendazole nanoliposomes in rats[J]. Chin J Hosp Pharm, 2017,37(8):702-706. (in Chinese) |
| ( 高惠静, 陈蓓, 张海波, 等. 阿苯达唑纳米脂质体冻干粉在大鼠体内药动学及肝靶向研究[J]. 中国医院药学杂志, 2017,37(8):702-706.) | |
| [6] | Wen H, Li HT. Advances in surgical operation and drug therapy for hepatic echinococcosis[J]. Chin Animal Health, 2017,19(7):29-32. (in Chinese) |
| ( 温浩, 李海涛. 肝包虫病的外科手术及药物治疗进展[J]. 中国动物保健, 2017,19(7):29-32.) | |
| [7] |
Samuel F, Degarege A, Erko B. Efficacy and side effects of albendazole currently in use against Ascaris, Trichuris and hookworm among school children in Wondo Genet, southern Ethiopia[J]. Parasitol Int, 2014,63(2):450-455.
doi: 10.1016/j.parint.2013.10.014 pmid: 24211489 |
| [8] | Wan MRQ. Protection of medicinal plant resources of Tibetan medicine in Qinghai[J]. J Clin Med Lit Electron, 2017,4(A2):20186-20187. (in Chinese) |
| ( 完玛仁青. 浅谈青海藏药药用植物资源保护[J]. 临床医药文献电子杂志, 2017,4(A2):20186-20187.) | |
| [9] | Dimaer DZPC. Jing Zhu Materia Medica[M]. Shanghai: Shanghai Science and Technology Press, 2012: 213. (in Chinese) |
| ( 帝玛尔·丹增彭措. 晶珠本草[M]. 上海: 上海科学技术出版社, 2012: 213.) | |
| [10] | Flora of China Editorial Committee of Chinese Academy of Science. The Flora of China[M]. Beijing: Science Press, 2014. (in Chinese) |
| ( 中国科学院中国植物志编辑委员会. 中国植物志[M]. 北京: 科学出版社, 2004.) | |
| [11] | Sun LP, Wang JR, Li XR, et al. Studies on the chemical constituents of Elsholtzia eriostachys(Elsholtzia eriostachys)ⅱ.isolation and identification of flavonoids constituents[J]. Chin Tradit Herb Drugs, 1997(11):646-648. (in Chinese) |
| ( 孙丽萍, 王建人, 李秀荣, 等. 黄花香薷化学成分的研究 Ⅱ. 黄酮类成分的分离和鉴定[J]. 中草药, 1997(11):646-648.) | |
| [12] | Xie P, Bai Y, Ci DJ, et al. Study on quality standard of the Tibetan Eriostachys elsholtzia[J]. Tibet Sci Technol, 2012(8):67-69. (in Chinese) |
| ( 谢平, 白央, 次德吉, 等. 藏药材黄花香薷的质量标准研究[J]. 西藏科技, 2012(8):67-69.) | |
| [13] | Liu XP, Jing XM. Research of chemical composition and biological activity of the essential oil from elsholtziaciliata[J]. J Heilongjiang August First Land Reclam Univ, 2018,30(3):35-39. (in Chinese) |
| ( 刘香萍, 敬雪敏. 香薷精油化学成分及其生物活性研究[J]. 黑龙江八一农垦大学学报, 2018,30(3):35-39.) | |
| [14] | Jiang S, Tang H, Xiao SG. Clinical application study of “Xiangru (Mosla herb)”[J]. Guid J Tradit Chin Med Pharmacol, 2015,21(9):95-97. (in Chinese) |
| ( 江岁, 唐华, 肖深根. 香薷的临床应用研究[J]. 中医药导报, 2015,21(9):95-97.) | |
| [15] | Li M, Miao MS. Characteristic analysis of the elsholtzia’s chemistry and pharmacology in clinical application[J]. Chin J Chin Med, 2015,30(4):578-579. (in Chinese) |
| ( 李敏, 苗明三. 香薷的化学、药理与临床应用特点分析[J]. 中医学报, 2015,30(4):578-579.) | |
| [16] | Dai XD, Ren YX, Liu X, et al. Transmission electron microscope investigation of Trichomonas vaginalis treated with Mosla chinensis Maxim[J]. J Trop Med, 2011,11(12):1379-1382. (in Chinese) |
| ( 戴晓冬, 任一鑫, 刘欣, 等. 香薷体外抗阴道毛滴虫的透射电镜观察[J]. 热带医学杂志, 2011,11(12):1379-1382.) | |
| [17] | Zheng LL, Cui Y, Qin YH, et al. Effect of Mosla chinensis Maxim on Trichomonas vaginalis in vitro[J]. J Dalian Med Univ, 2009,31(3):282-285. (in Chinese) |
| ( 郑莉莉, 崔昱, 秦元华, 等. 中药香薷体外杀灭阴道毛滴虫效果的观察[J]. 大连医科大学学报, 2009,31(3):282-285.) | |
| [18] | Liu HD, Wang HB, Fan HN, et al. Alveolar echinococcosis and immune evasion[J]. Chin J Parasitol Parasit Dis, 2018,36(6):655-660. (in Chinese) |
| ( 刘寒冬, 王宏宾, 樊海宁, 等. 多房棘球蚴病的免疫逃避机制[J]. 中国寄生虫学与寄生虫病杂志, 2018,36(6):655-660.) | |
| [19] | Hou XL, Li LH, Li L, et al. Changes in subsets and functional exhaustion of CD4+ T cells in spleens of mice infected with Echinococcus multilocularis [J]. Chin J Parasitol Parasit Dis Dec, 2020,38(5):611-618, 624. (in Chinese) |
| ( 侯昕伶, 李玲慧, 李亮, 等. 多房棘球蚴感染小鼠脾CD4+ T细胞亚群及其功能耗竭的变化 [J]. 中国寄生虫学与寄生虫病杂志, 2020,38(5):611-618, 624.) | |
| [20] | Mills SE. Practical histology for pathologists[M]. Xue DB, Chen J, Wang W (trans.). Beijing: Beijing Science and Technology Press, 2016: 23. (in Chinese) |
| ( Mills SE. 病理医师实用组织学[M]. 薛德彬, 陈健, 王炜, 译. 北京: 北京科学技术出版社, 2016: 23.) | |
| [21] | Qin FY, Song HT, Zhang X, et al. Research progress in the role of profilin in parasitic infection and immunity[J]. Chin J Parasitol Parasit Dis, 2019,37(6):709-712. (in Chinese) |
| ( 秦飞宇, 宋海桐, 张昕, 等. 抑制蛋白在寄生虫感染与免疫中的研究进展[J]. 中国寄生虫学与寄生虫病杂志, 2019,37(6):709-712.) | |
| [23] | Jiang JQ, E EDMT, Bao HE, et al. Correlation between eosinophils and immunity to parasitic infection[J]. Heilongjiang Animal Sci Vet Med, 2016(2):63-67. (in Chinese) |
| ( 姜建强, 额尔敦木图, 包花尔, 等. 嗜酸性粒细胞与寄生虫感染免疫的相关性[J]. 黑龙江畜牧兽医, 2016(3):63-67.) | |
| [24] | Li HW, Yang YR. Research progress in the mechanism of Echinococcus evasion[J]. Immunol J, 2010,26(11):1000-1002. (in Chinese) |
| ( 李红卫, 杨玉荣. 棘球蚴逃避或抑制宿主免疫系统清除作用的机制研究进展[J]. 免疫学杂志, 2010,26(11):1000-1002.) | |
| [25] | Huang ZK, Li JM. Macrophage polarization and its role in infectious diseases[J]. Int J Immunol, 2012,35(4):255-258, 281. (in Chinese) |
| ( 黄自坤, 李俊明. 巨噬细胞极化及其在感染性疾病中的作用[J]. 国际免疫学杂志, 2012,35(4):255-258, 281.) | |
| [26] | Yao Y, Xu J, Huang GX, et al. Research progress of Moslae Herba and predictive analysis on its Q-marker[J]. Chin Tradit Herb Drugs, 2020,51(10):2661-2670. (in Chinese) |
| ( 姚奕, 许浚, 黄广欣, 等. 香薷的研究进展及其质量标志物预测分析[J]. 中草药, 2020,51(10):2661-2670.) | |
| [27] | Yang S, Xu YQ, Xing YY, et al. Research advances on effects of plant-based flavonoids on immune and antioxidative functions in animals[J]. Chin J Animal Nutr, 2019,31(7):2958-2964. (in Chinese) |
| ( 杨硕, 徐元庆, 邢媛媛, 等. 植物源黄酮类化合物对动物免疫和抗氧化功能影响的研究进展[J]. 动物营养学报, 2019,31(7):2958-2964.) |
| [1] | LI Benfu, YANG Jing, YANG Jinyu, LUO Ruijuan, ZHU Binlin, CHEN Tailin, ZHANG Lijuan, LI Xueyao, YAN Xinliu, ZI Jinrong, PENG Jia, WANG Zhengqing, LI Jianxiong, CAI Xuan, XU Qian, WU Fangwei, YANG Yaming. Epidemiological investigation and case retrospective analysis of echinococcosis in Dali Prefecture, Yunnan Province [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(5): 573-578. |
| [2] | NI Bixian, XU Xiangzhen, ZHANG Qiang, TANG Feng, ZHANG Jiayao, MAO Fanzhen, DAI Yang, LIU Yaobao, CAO Jun. Epidemiological characteristics of echinococcosis cases reported in the National Notifiable Disease Report System in Jiangsu Province, 2015—2022 [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(5): 636-639. |
| [3] | FENG Xiaoxiao, BAIMA Yangjin, ZHANG Ting, LU Haojie, WEI Liming. Applied research of serum IgG sialylation modification in the diagnosis of hepatic echinococcosis [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(4): 434-439. |
| [4] | ZHU Aiya, WANG Xu, WANG Jiangyou, WANG Ying, LI Yang, SONG Shan, GENG Yan, LAN Ziyao, DAI Jiarui. A child case of alveolar echinococcosis in Guizhou Province [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(4): 520-523. |
| [5] | RAOWAN Tuolehong, ABUDUSALAMU Abulikemu, YANG Lingfei, CHEN Lu, LI Zhao, JIA Fang, SONG Tao. Effect evaluation and factor analysis of ultrasonic manifestations in the diagnosis of hepatic alveolar echinococcosis [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(3): 312-318. |
| [6] | WANG Wei, CAI Huixia. Surveillance of echinococcosis in Qinghai Province in 2020 [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(3): 319-324. |
| [7] | GUO Gang, REN Yuan, JIAO Hongjie, WU Juan, GUO Baoping, QI Wenjing, LI Jun, ZHANG Wenbao. Effect of intraperitoneal inoculation with Echinococcus microcysts on the infection and pathogenicity of E. multilocularis in mouse liver [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(2): 156-162. |
| [8] | LU Weimin, YANG Xiaotao, ZHU Ying, ZHANG Hong, LI Jiwei, WANG Yanchun. A child case of pulmonary cystic echinococcosis [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(2): 253-256. |
| [9] | MA Bingcun, LIU Yuying, ZHANG Tiantian, LEI Wen, MA Xiao, LIU Shou. A case-control study on the influencing factors of echinococcosis in Qinghai Province [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(2): 183-191. |
| [10] | KUI Yan, XUE Chuizhao, WANG Xu, LIU Baixue, WANG Ying, WANG Liying, YANG Shijie, HAN Shuai, WU Weiping, XIAO Ning. Progress of echinococcosis control in China, 2021 [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(2): 142-148. |
| [11] | MA Hui, CHONG Shigui, CHEN Gen, ZHANG Linghui, QIN Junmei, ZHAO Yumin. Research progress on the cellular signal pathways associated in alveolar echinococcosis [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(2): 223-227. |
| [12] | CAO Deping, WU Defang, PANG Mingquan, PENG Xiaohong, LI Dayu, FAN Haining. Difference analysis of the gut microbiome in patients with echinococcosis [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(1): 103-107. |
| [13] | DU Tao, HU Chunhui, GAN Xuehui, GAO Pan, ZHANG Fabin. Anti-Echinococcus multilocularis effect of total alkaloids of Sophora moorcroftiana in water solution and tablet forms in vitro and in vivo [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(1): 15-22. |
| [14] | WU Xiang-lin, YAN Fang, DUAN Hong-ju, QI Rong-ting, MA Tian-bo, GAO Jian-wei. Echinococcus multilocularis infection in dogs and other wild hosts in endemic area of Ningxia in 2021 [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2022, 40(6): 717-722. |
| [15] | LIU Yu-ying, ZHANG Tian-tian, MA Xiao, LEI Wen, MA Bing-cun, LIU Shou. Awareness and influencing factors of knowledge on echinococcosis prevention and control among adults in Qinghai Province [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2022, 40(6): 723-729. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||