
CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES ›› 2024, Vol. 42 ›› Issue (1): 48-54.doi: 10.12140/j.issn.1000-7423.2024.01.007
• ORIGINAL ARTICLES • Previous Articles Next Articles
ZHENG Guangfu1( ), LIU Xianbing1, JIANG Yuzhu1, LI Xinyu2, HU Xuemei1, ZHANG Haixia1,*(
), LIU Xianbing1, JIANG Yuzhu1, LI Xinyu2, HU Xuemei1, ZHANG Haixia1,*( )
)
Received:2023-07-31
Revised:2023-09-20
Online:2024-02-28
Published:2024-03-12
Contact:
*E-mail: Supported by:CLC Number:
ZHENG Guangfu, LIU Xianbing, JIANG Yuzhu, LI Xinyu, HU Xuemei, ZHANG Haixia. Imvolvement of placental neutrophils and IL-17 in adverse pregnancy outcome caused by Toxoplasma gondii infection in pregnant mice[J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2024, 42(1): 48-54.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.jsczz.cn/EN/10.12140/j.issn.1000-7423.2024.01.007
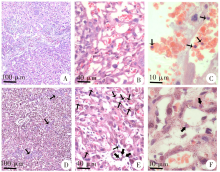
Fig. 2
Pathological section of placental tissue of pregnant mice with T. gondii infection (HE staining) A-C: Uninfected group, the placental tissue structure was normal without inflammatory foci (A, × 40), no inflammatory cell infiltration was observed in the labyrinth (B, × 100), and a small number of white blood cells were found mainly in blood vessels (C, × 400); D-F: T. gondii-infected group, inflammatory foci was observed (arrow) (D, × 40), polymorphonuclear granulocytes were seen in the labyrinth (arrow) (E, × 100), polymorphonuclear granulocytes infiltrating into the mesenchyma of the labyrinth (arrow) (F, × 400).
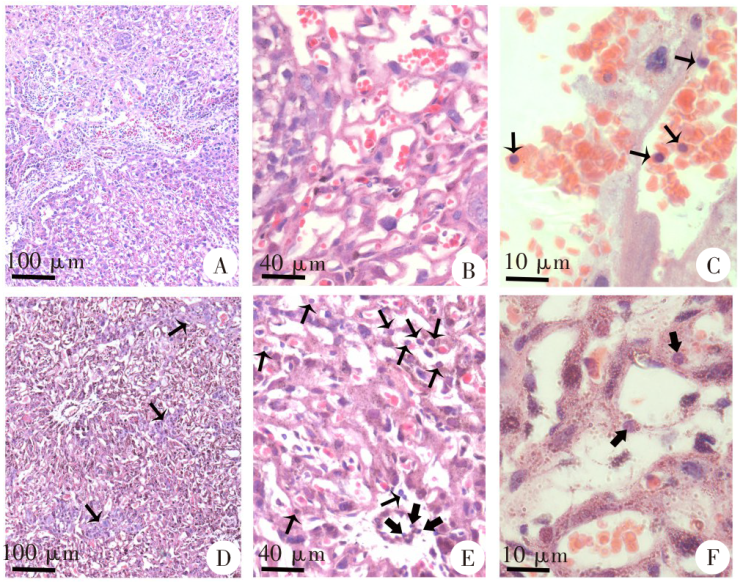

Fig. 3
The distribution of T. gondii in the placental tissue of infected pregnant mice (immunohistochemical staining) A: Blank control (× 100); B: Placental tissue of uninfected pregnant mice (× 100); C: T. gondii was scattered in the placental tissue of infected pregnant mice (× 100), small window for local magnification, indicating a RH tachyzoite (× 400); D: T. gondii mainly concentrated in the cells (× 100); E: The nuclei of T. gondii-concentrated cells showed polymorphic morphology (× 400).
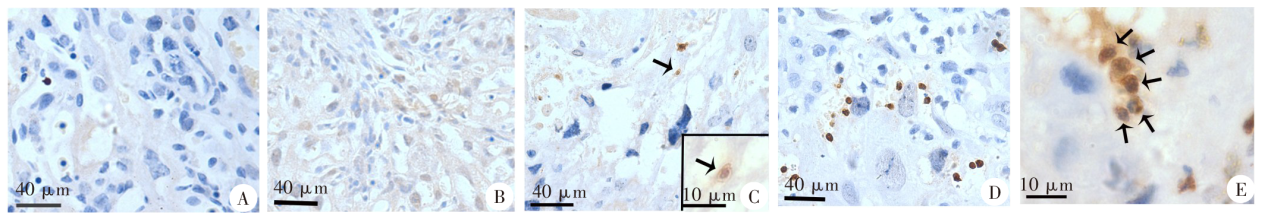

Fig. 5
The IL-17 expression level in the placental tissue of the pregnant mice infected with T. gondii (immunohistochemical staining, × 400) A: Blank control, no IL-17 positive expression cells; B: Uninfected group, small amount of positive expression of IL-17 and circular IL-17 positive cells; C: Infected group, increased expression of IL-17 positive cells near the blood vessel wall.
| [1] |
Tenter AM, Heckeroth AR, Weiss LM. Toxoplasma gondii: from animals to humans[J]. Int J Parasitol, 2000, 30(12/13): 1217-1258.
doi: 10.1016/S0020-7519(00)00124-7 |
| [2] | Wang ZD, Liu HH, Ma ZX, et al. Toxoplasma gondii infection in immunocompromised patients: a systematic review and meta-analysis[J]. Front Microbiol, 2017, 8:389. |
| [3] |
Veenstra van Nieuwenhoven AL, Heineman MJ, Faas MM. The immunology of successful pregnancy[J]. Hum Reprod Update, 2003, 9(4): 347-357.
doi: 10.1093/humupd/dmg026 pmid: 12926528 |
| [4] |
Pappas G, Roussos N, Falagas ME. Toxoplasmosis snapshots: global status of Toxoplasma gondii seroprevalence and implications for pregnancy and congenital toxoplasmosis[J]. Int J Parasitol, 2009, 39(12): 1385-1394.
doi: 10.1016/j.ijpara.2009.04.003 |
| [5] |
Pan M, Lyu CC, Zhao JL, et al. Sixty years (1957—2017) of research on toxoplasmosis in China: an overview[J]. Front Microbiol, 2017, 8: 1825.
doi: 10.3389/fmicb.2017.01825 |
| [6] |
Rowe JH, Ertelt JM, Xin LJ, et al. Regulatory T cells and the immune pathogenesis of prenatal infection[J]. Reproduction, 2013, 146(6): R191-R203.
doi: 10.1530/REP-13-0262 |
| [7] |
Zhao SJ, Muyayalo KP, Luo J, et al. Next generation of immune checkpoint molecules in maternal-fetal immunity[J]. Immunol Rev, 2022, 308(1): 40-54.
doi: 10.1111/imr.v308.1 |
| [8] |
Robbins JR, Bakardjiev AI. Pathogens and the placental fortress[J]. Curr Opin Microbiol, 2012, 15(1): 36-43.
doi: 10.1016/j.mib.2011.11.006 pmid: 22169833 |
| [9] |
Yarovinsky F. Innate immunity to Toxoplasma gondii infection[J]. Nat Rev Immunol, 2014, 14(2): 109-121.
doi: 10.1038/nri3598 pmid: 24457485 |
| [10] |
Burn GL, Foti A, Marsman G, et al. The neutrophil[J]. Immunity, 2021, 54(7): 1377-1391.
doi: 10.1016/j.immuni.2021.06.006 pmid: 34260886 |
| [11] |
Bliss SK, Gavrilescu LC, Alcaraz A, et al. Neutrophil depletion during Toxoplasma gondii infection leads to impaired immunity and lethal systemic pathology[J]. Infect Immun, 2001, 69(8): 4898-4905.
pmid: 11447166 |
| [12] |
Giaglis S, Stoikou M, Sur Chowdhury C, et al. Multimodal regulation of NET formation in pregnancy: progesterone antagonizes the pro-NETotic effect of estrogen and G-CSF[J]. Front Immunol, 2016, 7:565.
pmid: 27994595 |
| [13] |
Girardi G, Berman J, Redecha P, et al. Complement C5a receptors and neutrophils mediate fetal injury in the antiphospholipid syndrome[J]. J Clin Invest, 2003, 112(11): 1644-1654.
pmid: 14660741 |
| [14] |
Giaglis S, Stoikou M, Grimolizzi F, et al. Neutrophil migration into the placenta: good, bad or deadly?[J]. Cell Adh Migr, 2016, 10(1/2): 208-225.
doi: 10.1080/19336918.2016.1148866 |
| [15] |
Kelly MN, Kolls JK, Happel K, et al. Interleukin-17/interleukin-17 receptor-mediated signaling is important for generation of an optimal polymorphonuclear response against Toxoplasma gondii infection[J]. Infect Immun, 2005, 73(1): 617-621.
doi: 10.1128/IAI.73.1.617-621.2005 |
| [16] |
Nakashima A, Ito M, Shima T, et al. Accumulation of IL-17-positive cells in decidua of inevitable abortion cases[J]. Am J Reprod Immunol, 2010, 64(1):4-11.
doi: 10.1111/aji.2010.64.issue-1 |
| [17] |
Zhang HX, Hu XM, Liu XB, et al. The Treg/Th17 imbalance in Toxoplasma gondii-infected pregnant mice[J]. Am J Reprod Immunol, 2012, 67(2): 112-121.
doi: 10.1111/aji.2011.67.issue-2 |
| [18] |
Denison FC, Roberts KA, Barr SM, et al. Obesity, pregnancy, inflammation, and vascular function[J]. Reproduction, 2010, 140(3): 373-385.
doi: 10.1530/REP-10-0074 pmid: 20215337 |
| [19] |
Goldstein JA, Gallagher K, Beck C, et al. Maternal-fetal inflammation in the placenta and the developmental origins of health and disease[J]. Front Immunol, 2020, 11: 531543.
doi: 10.3389/fimmu.2020.531543 |
| [20] | Xue CL. Diagnosis, treatment and prevention of Toxoplasma gondii infection during pregnancy[J]. Chin J Parasitol Parasit Dis, 2000, 18(1): 55-57. (in Chinese) |
| (薛纯良. 孕期弓形虫感染的诊断、治疗和预防[J]. 中国寄生虫学与寄生虫病杂志, 2000, 18(1): 55-57.) | |
| [21] | Jiang SS, Yang HY, Jin N, et al. Relationship between TGF-β1/Smad3 signaling pathway and adverse pregnancy outcomes caused by Toxoplasma gondii infection[J]. Chin J Nosocomiol, 2023, 33(13): 2042-2046. (in Chinese) |
| (姜姗姗, 杨洪艳, 金男, 等. TGF-β1/Smad3信号通路与弓形虫感染孕妇不良妊娠结局的关系[J]. 中华医院感染学杂志, 2023, 33(13): 2042-2046.) | |
| [22] |
Kim CJ, Romero R, Chaemsaithong P, et al. Acute chorioamnionitis and funisitis: definition, pathologic features, and clinical significance[J]. Am J Obstet Gynecol, 2015, 213(4 Suppl): S29-S52.
doi: 10.1016/j.ajog.2015.08.040 |
| [23] | Zhong H, Jin XL, Jiang YF, et al. Expression of immune cells in placenta of pregnant women with pregnancy induced hypertension and its relationship with adverse pregnancy outcome[J]. J N Sichuan Med Coll, 2023, 38(3): 354-357. (in Chinese) |
| (钟辉, 晋兴林, 蒋玉芬, 等. 妊娠高血压综合征产妇胎盘组织中免疫细胞表达水平及其与不良妊娠结局的相关性[J]. 川北医学院学报, 2023, 38(3): 354-357.) | |
| [24] |
Ander SE, Diamond MS, Coyne CB. Immune responses at the maternal-fetal interface[J]. Sci Immunol, 2019, 4(31): eaat6114.
doi: 10.1126/sciimmunol.aat6114 |
| [25] |
Chaturvedi V, Ertelt JM, Jiang TT, et al. CXCR3 blockade protects against Listeria monocytogenes infection-induced fetal wastage[J]. J Clin Invest, 2015, 125(4): 1713-1725.
doi: 10.1172/JCI78578 pmid: 25751061 |
| [26] |
Aluvihare VR, Kallikourdis M, Betz AG. Regulatory T cells mediate maternal tolerance to the fetus[J]. Nat Immunol, 2004, 5(3): 266-271.
doi: 10.1038/ni1037 pmid: 14758358 |
| [27] |
Collins MK, Tay CS, Erlebacher A. Dendritic cell entrapment within the pregnant uterus inhibits immune surveillance of the maternal/fetal interface in mice[J]. J Clin Invest, 2009, 119(7): 2062-2073.
doi: 10.1172/JCI38714 pmid: 19546507 |
| [28] |
Chtanova T, Schaeffer M, Han SJ, et al. Dynamics of neutrophil migration in lymphnodesduring infection[J]. Immunity, 2008, 29(3): 487-496.
doi: 10.1016/j.immuni.2008.07.012 pmid: 18718768 |
| [29] | Miranda FJB, Rocha BC, Pereira MCA, et al. Toxoplasma gondii-induced neutrophil extracellular traps amplify the innate and adaptive response[J]. mBio, 2021, 12(5): e0130721. |
| [30] |
Nakashima A, Ito M, Yoneda S, et al. Circulating and decidual Th17 cell levels in healthy pregnancy[J]. Am J Reprod Immunol, 2010, 63(2): 104-109.
doi: 10.1111/aji.2010.63.issue-2 |
| [31] |
Pongcharoen S, Niumsup P, Sanguansermsri D, et al. The effect of interleukin-17 on the proliferation and invasion of JEG-3 human choriocarcinoma cells[J]. Am J Reprod Immunol, 2006, 55(4): 291-300.
pmid: 16533341 |
| [1] | XIE Xiaoman, SUN Hang, DAI Lisha, ZHU Wenju, WANG Lilei, XIE Huanhuan, DONG Hongjie, ZHANG Junmei, WANG Qi, ZHOU Beibei, ZHAO Guihua, XU Chao, YIN Kun. Effect of Toxoplasma gondii infection on m6A methylation modification of transcripts in mice brain tissue [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2024, 42(1): 27-35. |
| [2] | XUE Yushan, LIN Ping, CHENG Xunjia, FENG Meng. Damage caused by chronic infection of Toxoplasma gondii on the host central nervous system and its mechanism [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(5): 527-531. |
| [3] | JIANG Wenjing, MENG Yali, ZHAO Lina, WANG Chunmiao, ZHANG Xiaolei. Immunoprotection of nuclei acid vaccine dual-targeting rhoptry protein 18 and surface antigen 30 of Toxoplasma gondii in mice [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(5): 532-538. |
| [4] | ZHAO Ziqi, LV Fangli. Study on the inhibitory effect of artemether liposome on Toxoplasma gondii proliferation in vitro [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(4): 446-451. |
| [5] | ZHANG Chi, CHEN Jiating, XIN Zixuan, YANG Lili, YANG Zihan, PENG Hongjuan. Transcriptome analysis of mice brain chronically infected with Toxoplasma gondii and validation of the kynurenine pathway associated with depression [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(3): 270-278. |
| [6] | OU Yangran, LIU Xingzhuo, HUANG Shiguang, LYU Fangli. Effect of locking galectin-receptor interaction on the immunopathology of small intestine of Toxoplasma gondii-infected mice [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(3): 279-285. |
| [7] | DU Juan, LI Jia, WU Di, YU Qi, ZHANG Wei, BAI Runian, GUO Junlin, LIU Qingbin, LEI Qili, GU Chuanhui, WANG Meng, ZHAO Haojun. Seroepidemiological survey of Toxoplasma gondii infection in dogs and cats in Beijing 2022 [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(3): 389-392. |
| [8] | LI Chang, DU Xinyue, YAN Min, WANG Zhaojun. Research advances on the role and mechanism of neutrophil extracellular traps in parasitic infection [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(2): 219-222. |
| [9] | LI Jia-ming, WANG Yi-xuan, YANG Ning-ai, MA Hui-hui, LAN Min, LIU Chun-lan, ZHAO Zhi-jun. Effects of ROP16 protein of Toxoplasma gondii on polarization and apoptosis of MH-S cells and their related mechanisms [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2022, 40(5): 579-586. |
| [10] | ZOU Wei-hao, WU Wei-ling, LIAO Yuan-peng, CHEN Min, PENG Hong-juan. Preparation and application of monoclonal antibody against Toxoplasma gondii bradyzoite antigen 1 [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2022, 40(5): 587-593. |
| [11] | DAI Li-sha, ZHANG Li-xin, YIN Kun. Research advances in Toxoplasma gondii induced host mental-behavioural disorders [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2022, 40(5): 642-646. |
| [12] | HUANG Yuan-yuan, YAO Shi-jie, BIAN Zhi-fang, WEN Yi-xin, ZHENG Li, CAO Ya-ming. Immunoprotective effect of dexamethasone on experimental cerebral malaria in mice [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2022, 40(4): 446-453. |
| [13] | WANG Jie, WEN Hong-yang, CHEN Ying, AN Ran, LUO Qing-li, SHEN Ji-long, DU Jian. Construction and identification of macrophage migration inhibitory factor gene knockout strain of Toxoplasma gondii [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2022, 40(3): 349-354. |
| [14] | WANG Zhen-xun, XIONG Si-si, SUN Xia-hui, WANG Yong-liang, PAN Ge, HE Shen-yi, CONG Hua. Differential expression and action mechanism of lncRNA102796 in the brain of mice with chronic infection of Toxoplasma gondii [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2022, 40(2): 187-193. |
| [15] | JIANG Feng, CHEN Run, DU Ning-ning, ZHU Meng-yi, ZHONG Hao, CHEN Hui, XI Xu-xia, ZHAN Xiao-dong, LI Chao-pin. Investigation of Toxoplasma gondii infection in pet dogs and cats in Wuhu City [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2022, 40(1): 124-126. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||