
CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES ›› 2022, Vol. 40 ›› Issue (4): 446-453.doi: 10.12140/j.issn.1000-7423.2022.04.005
• ORIGINAL ARTICLES • Previous Articles Next Articles
HUANG Yuan-yuan( ), YAO Shi-jie, BIAN Zhi-fang, WEN Yi-xin, ZHENG Li, CAO Ya-ming*(
), YAO Shi-jie, BIAN Zhi-fang, WEN Yi-xin, ZHENG Li, CAO Ya-ming*( )
)
Received:2021-12-22
Revised:2022-04-02
Online:2022-08-30
Published:2022-09-07
Contact:
CAO Ya-ming
E-mail:1349759194@qq.com;ymccmu@163.com
Supported by:CLC Number:
HUANG Yuan-yuan, YAO Shi-jie, BIAN Zhi-fang, WEN Yi-xin, ZHENG Li, CAO Ya-ming. Immunoprotective effect of dexamethasone on experimental cerebral malaria in mice[J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2022, 40(4): 446-453.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.jsczz.cn/EN/10.12140/j.issn.1000-7423.2022.04.005

Fig. 3
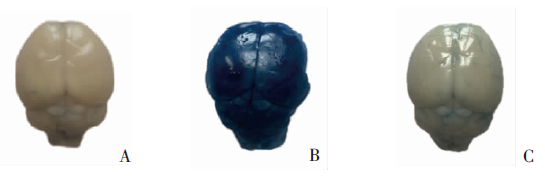
The effect of DEX treatment on BBB permeability in ECM mice(EB staining) A: Control group, the blood-brain barrier of the mice was not damaged, and the color of the brain tissue was normal; B: Infection group, the blood-brain barrier of the mice was severely damaged, EB infiltrated the brain tissue completely, and the brain tissue was dark blue; C: DEX treatment group, the blood-brain barrier of the mice was basically intact, with only a small amount of EB infiltrated into the brain tissue.
| [1] |
Cain DW, Cidlowski JA. Specificity and sensitivity of glucocorticoid signaling in health and disease[J]. Best Pract Res Clin Endocrinol Metab, 2015, 29(4): 545-556.
doi: 10.1016/j.beem.2015.04.007 |
| [2] |
Cain DW, Cidlowski JA. Immune regulation by glucocorticoids[J]. Nat Rev Immunol, 2017, 17(4): 233-247.
doi: 10.1038/nri.2017.1 |
| [3] | Mahase E. Covid-19: low dose steroid cuts death in ventilated patients by one third, trial finds[J]. BMJ, 2020, 369: m2422. |
| [4] |
Ledford H. Coronavirus breakthrough: dexamethasone is first drug shown to save lives[J]. Nature, 2020, 582(7813): 469.
doi: 10.1038/d41586-020-01824-5 |
| [5] |
He X, Ashbrook AW, Du Y, et al. RTP4 inhibits IFN-I response and enhances experimental cerebral malaria and neuropathology[J]. Proc Natl Acad Sci USA, 2020, 117(32): 19465-19474.
doi: 10.1073/pnas.2006492117 |
| [6] |
Hai L, Shi XY, Wang Q. Attenuated T cell responses are associated with the blockade of cerebral malaria development by YOP1-deficient Plasmodium berghei ANKA[J]. Front Immunol, 2021, 12: 642585.
doi: 10.3389/fimmu.2021.642585 |
| [7] |
Wang J, Li Y, Shen Y, et al. PDL1 fusion protein protects against experimental cerebral malaria via repressing over-reactive CD8+ T cell responses[J]. Front Immunol, 2019, 9: 3157.
doi: 10.3389/fimmu.2018.03157 |
| [8] |
Van den Steen PE, Geurts N, Deroost K, et al. Immunopathology and dexamethasone therapy in a new model for malaria-associated acute respiratory distress syndrome[J]. Am J Respir Crit Care Med, 2010, 181(9): 957-968.
doi: 10.1164/rccm.200905-0786OC |
| [9] |
Moreira DR, Uberti ACMG, Gomes ARQ, et al. Dexamethasone increased the survival rate in Plasmodium berghei-infected mice[J]. Sci Rep, 2021, 11: 2623.
doi: 10.1038/s41598-021-82032-7 pmid: 33514836 |
| [10] |
Curfs JH, Schetters TP, Hermsen CC, et al. Immunological aspects of cerebral lesions in murine malaria[J]. Clin Exp Immunol, 1989, 75(1): 136-140.
pmid: 2649283 |
| [11] | Liu TP, Fu Y, Xu WY. Immunopathological mechanism of cerebral malaria[J]. Chin J Parasitol Parasit Dis, 2011, 29(1): 64-67. (in Chinese) |
| ( 刘太平, 付雍, 徐文岳. 脑型疟发生的免疫病理机制[J]. 中国寄生虫学与寄生虫病杂志, 2011, 29(1): 64-67.) | |
| [12] |
Campanella GSV, Tager AM, El Khoury JK, et al. Chemokine receptor CXCR3 and its ligands CXCL9 and CXCL10 are required for the development of murine cerebral malaria[J]. Proc Natl Acad Sci USA, 2008, 105(12): 4814-4819.
doi: 10.1073/pnas.0801544105 |
| [13] |
van der Heyde HC, Nolan J, Combes V, et al. A unified hypothesis for the genesis of cerebral malaria: sequestration, inflammation and hemostasis leading to microcirculatory dysfunction[J]. Trends Parasitol, 2006, 22(11): 503-508.
doi: 10.1016/j.pt.2006.09.002 |
| [14] |
Shikani HJ, Freeman BD, Lisanti MP, et al. Cerebral malaria[J]. Am J Pathol, 2012, 181(5): 1484-1492.
doi: 10.1016/j.ajpath.2012.08.010 pmid: 23021981 |
| [15] |
Burrack KS, Huggins MA, Taras E, et al. Interleukin-15 complex treatment protects mice from cerebral malaria by inducing interleukin-10-producing natural killer cells[J]. Immunity, 2018, 48(4): 760-772.e4.
doi: 10.1016/j.immuni.2018.03.012 |
| [16] |
Simhadri PK, Malwade R, Vanka R, et al. Dysregulation of LIMK-1/cofilin-1 pathway: a possible basis for alteration of neuronal morphology in experimental cerebral malaria[J]. Ann Neurol, 2017, 82(3): 429-443.
doi: 10.1002/ana.25028 pmid: 28843047 |
| [17] |
Howland SW, Poh CM, Gun SY, et al. Brain microvessel cross-presentation is a hallmark of experimental cerebral malaria[J]. EMBO Mol Med, 2013, 5(7): 984-999.
doi: 10.1002/emmm.201202273 |
| [18] |
Vandermosten L, Pham TT, Knoops S, et al. Adrenal hormones mediate disease tolerance in malaria[J]. Nat Commun, 2018, 9: 4525.
doi: 10.1038/s41467-018-06986-5 pmid: 30375380 |
| [19] |
Rungruang T, Klosek SK. Chronic steroid administration does not suppress Plasmodium development and maturation[J]. Parasitol Res, 2007, 101(4): 1091-1095.
doi: 10.1007/s00436-007-0592-x |
| [20] |
Giles AJ, Hutchinson MKND, Sonnemann HM, et al. Dexamethasone-induced immunosuppression: mechanisms and implications for immunotherapy[J]. J Immunother Cancer, 2018, 6(1): 51.
doi: 10.1186/s40425-018-0371-5 |
| [21] |
Xia M, Gasser J, Feige U. Dexamethasone enhances CTLA-4 expression during T cell activation[J]. Cell Mol Life Sci, 1999, 55(12): 1649-1656.
pmid: 10526580 |
| [22] |
Keir ME, Francisco LM, Sharpe AH. PD-1 and its ligands in T-cell immunity[J]. Curr Opin Immunol, 2007, 19(3): 309-314.
doi: 10.1016/j.coi.2007.04.012 |
| [23] |
Xing KL, Gu BX, Zhang P, et al. Dexamethasone enhances programmed cell death 1 (PD-1) expression during T cell activation: an insight into the optimum application of glucocorticoids in anti-cancer therapy[J]. BMC Immunol, 2015, 16(1): 39.
doi: 10.1186/s12865-015-0103-2 |
| [24] | Wang J, Shen Y, Li Y, et al. Recent progress in immune checkpoint molecules in Plasmodium infection and immunity[J]. Chin J Parasitol Parasit Dis, 2019, 37(4): 472-480. (in Chinese) |
| ( 王军, 沈燕, 李悦, 等. 免疫检查点分子调控在疟原虫感染与免疫中的研究进展[J]. 中国寄生虫学与寄生虫病杂志, 2019, 37(4): 472-480.) | |
| [25] |
Haque A, Best SE, Amante FH, et al. CD4+ natural regulatory T cells prevent experimental cerebral malaria via CTLA-4 when expanded in vivo[J]. PLoS Pathog, 2010, 6(12): e1001221.
doi: 10.1371/journal.ppat.1001221 |
| [26] |
Tabardel Y, Duchateau J, Schmartz D, et al. Corticosteroids increase blood interleukin-10 levels during cardiopulmonary bypass in men[J]. Surgery, 1996, 119(1): 76-80.
doi: 10.1016/S0039-6060(96)80217-0 |
| [27] | Li PY, Gao HW, Dong TW, et al. Effect of different sources of IL-10 on regulating immune pathology in mice infected with cerebral malaria[J]. J Harbin Med Univ, 2015, 49(4): 296-299, 304. (in Chinese) |
| ( 李培育, 高宏伟, 董天崴, 等. 不同来源的IL-10对脑疟小鼠免疫病理损伤的调控作用[J]. 哈尔滨医科大学学报, 2015, 49(4): 296-299, 304.) | |
| [28] |
Amici SA, Dong J, Guerau-de-Arellano M. Molecular mechanisms modulating the phenotype of macrophages and microglia[J]. Front Immunol, 2017, 8: 1520.
doi: 10.3389/fimmu.2017.01520 |
| [29] | Zhang LJ, Zhang JQ, You ZL. Switching of the microglial activation phenotype is a possible treatment for depression disorder[J]. Front Cell Neurosci, 2018, 12: 306. |
| [30] |
Biswas SK, Mantovani A. Macrophage plasticity and interaction with lymphocyte subsets: cancer as a paradigm[J]. Nat Immunol, 2010, 11(10): 889-896.
doi: 10.1038/ni.1937 |
| [31] |
Besnard AG, Guabiraba R, Niedbala W, et al. IL-33-mediated protection against experimental cerebral malaria is linked to induction of type 2 innate lymphoid cells, M2 macrophages and regulatory T cells[J]. PLoS Pathog, 2015, 11(2): e1004607.
doi: 10.1371/journal.ppat.1004607 |
| [1] | GONG Yanfeng, LI Zifen, TANG Guai, HUANG Meiqin, ZHOU Binghua, HU Qiang. Epidemiological characteristics of malaria in Jiangxi Province from 2015 to 2022 [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(5): 586-592. |
| [2] | WEI Luanting, LI Runze, GUAN Liangchao, ZHANG Qianyu, LI Cheng, CAO Yaming, ZHAO Yan. Research progress of antimalarial drugs [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(4): 486-491. |
| [3] | ZHANG Le, XIA Jiawei, LI Xiang, MA Zhongxu, JIANG Jianjie, TANG Yalin, LIU Shu, ZHANG Kaiyi. Clinical analysis of imported COVID-19 cases complicated with severe falciparum malaria [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(4): 506-509. |
| [4] | CAO Wei, WANG Yi, ZHANG Xizhi, TONG Guodong, YANG Chao, SHEN Yan, ZHAO Ya. Research progress in adjunctive therapy of cerebral malaria [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(3): 361-373. |
| [5] | GENG Yan, LAN Ziyao, LI Yang, DAI Jiarui, CAI Shan, LU Lidan, HUANG Yuting, SHI Weifang, SHE Danya. Epidemiological analysis of malaria in Guizhou Province from 2017 to 2021 [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(3): 384-388. |
| [6] | ZHANG Li, YI Boyu, YIN Jianhai, XIA Zhigui. Epidemiological characteristics of malaria in China, 2022 [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(2): 137-141. |
| [7] | CHEN Zhuyun, OUYANG Rong, XIAO Lizhen, LIN Yaoying, XIE Hanguo, ZHANG Shanying. Current status of the primary surveillance and response system during the post malaria elimination phase in Fujian Province [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(2): 170-175. |
| [8] | SUN Jun. The biological significance of malarial hemozoin’s formation [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(2): 209-212. |
| [9] | CHEN Zhihui, HONG Jing, ZHANG Rongbing, YANG Qian, YE Qing, LI Jianrong, TIAN Rong. Epidemiological analysis on malaria cases reported in Kunming during 2006—2021 [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(2): 233-237. |
| [10] | LIU Jiancheng, XU Yan, WANG Longjiang, KONG Xiangli, WANG Yongbin, LI Yuejin. Surveillance on imported malaria in Linyi City of Shandong Province from 2015 to 2021 [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(2): 249-252. |
| [11] | ZHANG Yaoguang, JIANG Li, WANG Zhenyu, ZHU Min, ZHU Qian, MA Xiaojiang, YU Qing, Chen Jian. Analysis of the causes of misdiagnosis of seven imported malaria cases in Shanghai from 2020 to 2021 [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(1): 68-74. |
| [12] | LI Su-hua, JI Peng-hui, ZHOU Rui-min, HE Zhi-quan, QIAN Dan, YANG Cheng-yun, LIU Ying, LU De-ling, WANG Hao, ZHANG Hong-wei, ZHAO Yu-ling. Appraisal of diagnosis capacity of malaria reference laboratories in Henan Province during 2015—2019 [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2022, 40(6): 748-753. |
| [13] | LI Mei, ZHOU He-jun, XIA Zhi-gui, ZHANG Li, TU Hong, YIN Jian-hai. Quality evaluation on the preparation of the malaria blood smears at the national level in 2019 [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2022, 40(6): 754-759. |
| [14] | ZHAO Hui, XIANG Zheng, ZHOU Long-can, PAN Mao-hua, YANG Zhao-qing. Research progress of amodiaquine as an antimalarial drug [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2022, 40(6): 786-791. |
| [15] | JI Peng-hui, JIANG Tian-tian, HE Zhi-quan, ZHOU Rui-min, LI Su-hua, YANG Cheng-yun, QIAN Dan, LIU Ying, WANG Hao, ZHANG Hong-wei. Analysis on epidemiological characteristics of imported quartan malaria in Henan Province from 2011 to 2021 [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2022, 40(6): 801-805. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||