
CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES ›› 2023, Vol. 41 ›› Issue (6): 691-698.doi: 10.12140/j.issn.1000-7423.2023.06.005
• ORIGINAL ARTICLES • Previous Articles Next Articles
HUA Lijuan1( ), LI Shenghao1, CHANG Guoji1, LIU Siqi1, DING Jie1, BAI Baoli1, ZHANG Lu2, WANG Qingqing1,*(
), LI Shenghao1, CHANG Guoji1, LIU Siqi1, DING Jie1, BAI Baoli1, ZHANG Lu2, WANG Qingqing1,*( )
)
Received:2023-06-12
Revised:2023-08-06
Online:2023-12-30
Published:2023-12-19
Contact:
* E-mail: Supported by:CLC Number:
HUA Lijuan, LI Shenghao, CHANG Guoji, LIU Siqi, DING Jie, BAI Baoli, ZHANG Lu, WANG Qingqing. Drug-regulation of PPAR-γ/RXR-α signal pathways on ameliorating lung injury induced by Paragonimus proliferus infection in rats[J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(6): 691-698.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.jsczz.cn/EN/10.12140/j.issn.1000-7423.2023.06.005

Fig. 1
Adult worms in the chest and lungs of rats infected with excysted metacercariae of P. proliferus A: Excysted metacercariae of P. proliferus isolated from freshwater crabs; B: Healthy control rats, the lung was normal; C, D: Infected rats, parasite cysts were found in the lung, and parasites were found in the thorax. The red arrow show parasite cysts formed in the lung, and the yellow arrows show parasitic worms.
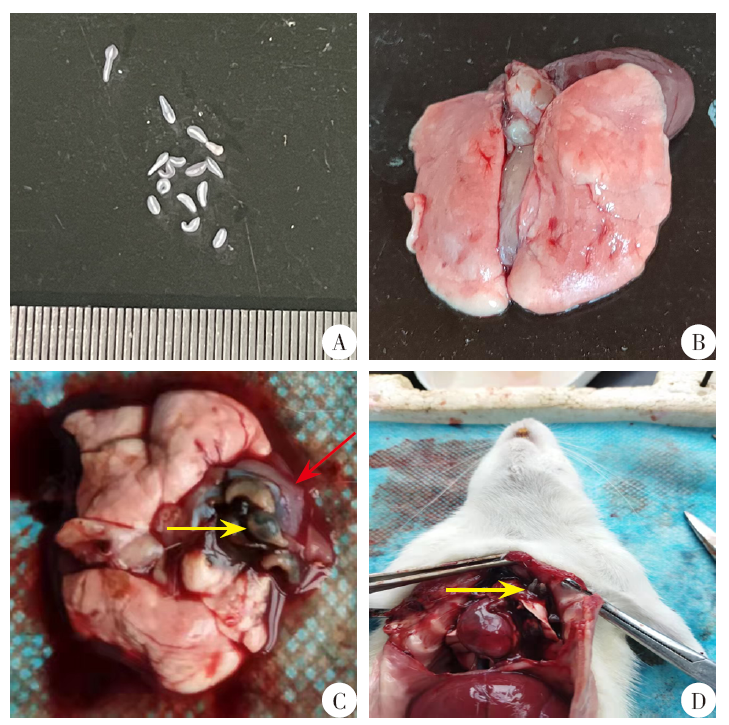

Fig. 2
Pathological changes in lung tissues of rats infected with excysted metacercariae of P. proliferus after drug treatment (HE staining, × 400) A: Healthy control group, the structure of the rat lung tissue was normal; B: Infection control group, a large number of inflammatory cells infiltrated in the alveolar interval, the alveolar wall was severely thickened, the alveolar cavities collapsed or closed (the yellow frame); C: High-fat diet group, a number of inflammatory cells infiltrate in the alveolar interval, the alveolar wall was thickened, the inflation of alveolar cavity iwas slightly improved compared with the infection control group; D, E: Rosiglitazone group and bexarotene group, compared with the nfection control group, the aggregation of inflammatory cells in the alveolar septum was significantly reduced, the degree of alveolar wall thickening was significantly reduced, and the alveolar cavity inflation was obviously improved.
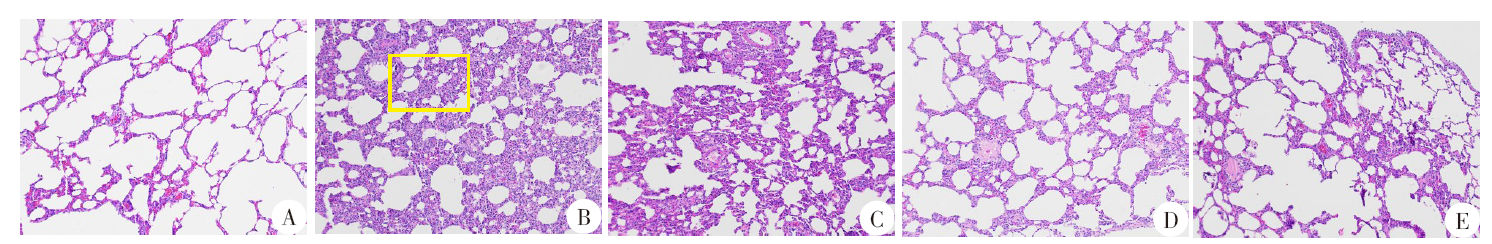

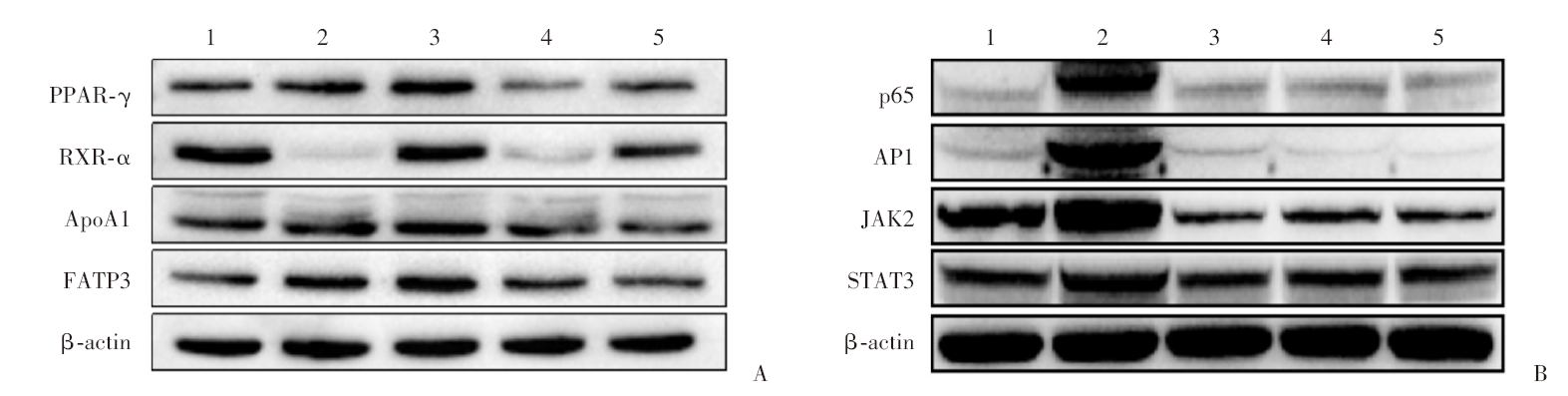
Fig. 3
Western blotting analysis of key target proteins of PPAR-γ/RXR-α(A), NF-κB and JAK-STAT(B)signaling pathways in lung tissue of rats infected with excysted metacercariae of P. proliferus after drug treatment 1: Healthy control group; 2: Infection control group; 3: High-fat diet group; 4: Rosiglitazone group; 5: Bexarotene group.
| [1] | Yao N. Expression and significance of IL-6 and IL-10 in lung inflammation of rats infected with Paragonimus proliferus[D]. Kunming: Kunming Medical University, 2014: 6. (in Chinese) |
| (姚娜. IL-6和IL-10在丰宫并殖吸虫所致大鼠肺部炎症中的表达及意义[D]. 昆明: 昆明医科大学, 2014: 6.) | |
| [2] | Li SH, Du YR, Wu KL, et al. Study on patterns of the Th1/Th2 immune response induced by Paragonimus proliferus infection in rats[J]. J Pathog Biol, 2021, 16(2): 171-176. (in Chinese) |
| (李生浩, 杜映荣, 武昆利, 等. 丰宫并殖吸虫感染诱导大鼠Th1/Th2免疫应答的偏移模式研究[J]. 中国病原生物学杂志, 2021, 16(2): 171-176.) | |
| [3] |
Egan TJ. Haemozoin formation[J]. Mol Biochem Parasitol, 2008, 157(2): 127-136.
doi: 10.1016/j.molbiopara.2007.11.005 |
| [4] |
Kim IS, Silwal P, Jo EK. Peroxisome proliferator-activated receptor-targeted therapies: challenges upon infectious diseases[J]. Cells, 2023, 12(4): 650.
doi: 10.3390/cells12040650 |
| [5] | Li SH. Mechanisms of successful parasitism and pathogenesis of paragonimiasis caused by Paragonimus proliferus in rats[D]. Kunming: Kunming Medical University, 2021: 63-68. (in Chinese) |
| (李生浩. 丰宫并殖吸虫成功寄生大鼠及致并殖吸虫病的机制研究[D]. 昆明: 昆明医科大学, 2021: 63-68.) | |
| [6] | Huan Y, Peng J, Pan X, et al. Updated research progress of selective PPARγ modulators[J]. Acta Pharm Sin, 2021, 56(2): 352-359. (in Chinese) |
| (环奕, 彭军, 潘璇, 等. 选择性PPARγ调节剂的研究新进展[J]. 药学学报, 2021, 56(2): 352-359.) | |
| [7] |
Szanto A, Nagy L. The many faces of PPARgamma: anti-inflammatory by any means?[J]. Immunobiology, 2008, 213(9/10): 789-803.
doi: 10.1016/j.imbio.2008.07.015 |
| [8] | Chan MM, Evans KW, Moore AR, et al. Peroxisome proliferator-activated receptor (PPAR): balance for survival in parasitic infections[J]. J Biomed Biotechnol, 2010, 2010: 828951. |
| [9] |
Serghides L, Patel SN, Ayi K, et al. Rosiglitazone modulates the innate immune response to Plasmodium falciparum infection and improves outcome in experimental cerebral malaria[J]. J Infect Dis, 2009, 199(10): 1536-1545.
doi: 10.1086/598222 pmid: 19392627 |
| [10] |
Tunctan B, Kucukkavruk SP, Temiz-Resitoglu M, et al. Bexarotene, a selective RXRα agonist, reverses hypotension associated with inflammation and tissue injury in a rat model of septic shock[J]. Inflammation, 2018, 41(1): 337-355.
doi: 10.1007/s10753-017-0691-5 pmid: 29188497 |
| [11] | Lin R, Li XM, Zhang HM. Experiment infection of rats with encysted metacercariae of Paragonimus heterotremus through hypodermic and muscle inoculation[J]. Guangxi J Prev Med, 2001, 7(4): 201-203. (in Chinese) |
| (林睿, 黎学铭, 张鸿满. 异盘并殖吸虫两种途径感染大鼠的实验观察[J]. 广西预防医学, 2001, 7(4): 201-203.) | |
| [12] | Chang GJ, Li N, Wang QQ, et al. Dynamic transcriptome landscape of pulmonary tissues of rats infected with Paragonimus proliferus[J]. Am J Transl Res, 2022, 14(5): 3395-3406. |
| [13] | Blair D. Paragonimiasis[M]// ToledoR, FriedB. Digenetic trematodes. Cham: Springer, 2019: 105-138. |
| [14] |
Yoshida A, Doanh PN, Maruyama H. Paragonimus and paragonimiasis in Asia: an update[J]. Acta Trop, 2019, 199: 105074.
doi: 10.1016/j.actatropica.2019.105074 |
| [15] |
Lam NS, Long XX, Su XZ, et al. Artemisinin and its derivatives in treating helminthic infections beyond schistosomiasis[J]. Pharmacol Res, 2018, 133: 77-100.
doi: S1043-6618(17)31042-3 pmid: 29727708 |
| [16] |
Qu ZX, Li F, Ma CD, et al. Effects of Gentiana scabra bage on expression of hepatic type Ⅰ, Ⅲ collagen proteins in Paragonimus skrjabini rats with liver fibrosis[J]. Asian Pac J Trop Med, 2015, 8(1): 60-63.
doi: 10.1016/S1995-7645(14)60188-7 |
| [17] |
Wang J, Luo L, Zhao XT, et al. Forsythiae Fructuse extracts alleviates LPS-induced acute lung injury in mice by regulating PPAR-γ/RXR-α in lungs and colons[J]. J Ethnopharmacol, 2022, 293: 115322.
doi: 10.1016/j.jep.2022.115322 |
| [18] |
Gallardo-Soler A, Gómez-Nieto C, Campo ML, et al. Arginase Ⅰ induction by modified lipoproteins in macrophages: a peroxisome proliferator-activated receptor-gamma/delta-mediated effect that links lipid metabolism and immunity[J]. Mol Endocrinol, 2008, 22(6): 1394-1402.
doi: 10.1210/me.2007-0525 pmid: 18323470 |
| [19] |
Chen KM, Peng CY, Shyu LY, et al. Peroxisome-proliferator activator receptor γ in mouse model with meningoencephalitis caused by Angiostrongylus cantonensis[J]. J Parasitol, 2021, 107(2): 205-213.
doi: 10.1007/s00436-010-1852-8 |
| [20] |
Chen H, He YW, Liu WQ, et al. Rosiglitazone prevents murine hepatic fibrosis induced by Schistosoma japonicum[J]. World J Gastroenterol, 2008, 14(18): 2905-2911.
doi: 10.3748/wjg.14.2905 |
| [21] |
Morichika D, Miyahara N, Fujii U, et al. A retinoid X receptor partial agonist attenuates pulmonary emphysema and airway inflammation[J]. Respir Res, 2019, 20(1): 2.
doi: 10.1186/s12931-018-0963-0 |
| [22] |
Fujii U, Miyahara N, Taniguchi A, et al. Effect of a retinoid X receptor partial agonist on airway inflammation and hyperresponsiveness in a murine model of asthma[J]. Respir Res, 2017, 18(1): 23.
doi: 10.1186/s12931-017-0507-z |
| [23] |
Xu CR, Chen HJ, Zhou SJ, et al. Pharmacological activation of RXR-α promotes hematoma absorption via a PPAR-γ-dependent pathway after intracerebral hemorrhage[J]. Neurosci Bull, 2021, 37(10): 1412-1426.
doi: 10.1007/s12264-021-00735-3 pmid: 34142331 |
| [24] | Philpott J, Kazimierczyk S, Korgaonkar P, et al. RXRα regulates the development of resident tissue macrophages[J]. Immuno Horizons, 2022, 6(6): 366-372. |
| [25] |
Certo M, Endo Y, Ohta K, et al. Activation of RXR/PPARγ underlies neuroprotection by bexarotene in ischemic stroke[J]. Pharmacol Res, 2015, 102: 298-307.
doi: 10.1016/j.phrs.2015.10.009 pmid: 26546745 |
| [26] |
Lee BR, Paing MH, Sharma-Walia N. Cyclopentenone prostaglandins: biologically active lipid mediators targeting inflammation[J]. Front Physiol, 2021, 12: 640374.
doi: 10.3389/fphys.2021.640374 |
| [27] |
Lê HG, Kang JM, Võ TC, et al. Naegleria fowleri cathepsin B induces a pro-inflammatory immune response in BV-2 microglial cells via NF-κB and AP-1 dependent-MAPK signaling pathway[J]. Int J Mol Sci, 2022, 23(15): 8388.
doi: 10.3390/ijms23158388 |
| [28] |
Uddin J, Garcia HH, Gilman RH, et al. Monocyte-astrocyte networks and the regulation of chemokine secretion in neurocysticercosis[J]. J Immunol, 2005, 175(5): 3273-3281.
pmid: 16116219 |
| [29] |
Penas FN, Carta D, Cevey ÁC, et al. Pyridinecarboxylic acid derivative stimulates pro-angiogenic mediators by PI3K/AKT/mTOR and inhibits reactive nitrogen and oxygen species and NF-κB activation through a PPARγ-dependent pathway in T. cruzi-infected macrophages[J]. Front Immunol, 2020, 10: 2955.
doi: 10.3389/fimmu.2019.02955 |
| [30] |
Bi J, Sun K, Wu H, et al. PPARγ alleviated hepatocyte steatosis through reducing SOCS3 by inhibiting JAK2/STAT3 pathway[J]. Biochem Biophys Res Commun, 2018, 498(4): 1037-1044.
doi: 10.1016/j.bbrc.2018.03.110 |
| [31] |
Yao JM, Zhao Y. Lp-PLA2 silencing ameliorates inflammation and autophagy in nonalcoholic steatohepatitis through inhibiting the JAK2/STAT3 pathway[J]. PeerJ, 2023, 11: e15639.
doi: 10.7717/peerj.15639 |
| [32] |
Cai YH, Chen H, Mo XW, et al. Toxoplasma gondii inhibits apoptosis via a novel STAT3-miR-17-92-Bim pathway in macrophages[J]. Cell Signal, 2014, 26(6): 1204-1212.
doi: 10.1016/j.cellsig.2014.02.013 |
| [33] | Qi RL, Huang JX, Yang FY, et al. Fatty acid transport protein family and their mediation in transmembrane transportation of fatty acids[J]. Chin J Anim Nutr, 2013, 25(5): 905-911. (in Chinese) |
|
(齐仁立, 黄金秀, 杨飞云, 等. 脂肪酸转运蛋白家族及其介导的脂肪酸跨膜转运[J]. 动物营养学报, 2013, 25(5): 905-911.)
doi: 10.3969/j.issn.1006-267x.2013.05.003 |
|
| [34] |
Stahl A. A current review of fatty acid transport proteins (SLC27)[J]. Pflugers Arch, 2004, 447(5): 722-727.
doi: 10.1007/s00424-003-1106-z |
| [35] |
Ahmad Y, Shukla D, Garg I, et al. Identification of haptoglobin and apolipoprotein A-I as biomarkers for high altitude pulmonary edema[J]. Funct Integr Genomics, 2011, 11(3): 407-417.
doi: 10.1007/s10142-011-0234-3 |
| [36] |
Lee EH, Lee EJ, Kim HJ, et al. Overexpression of apolipoprotein A1 in the lung abrogates fibrosis in experimental silicosis[J]. PLoS One, 2013, 8(2): e55827.
doi: 10.1371/journal.pone.0055827 |
| [37] |
Paul S, Gangwar A, Bhargava K, et al. D4F prophylaxis enables redox and energy homeostasis while preventing inflammation during hypoxia exposure[J]. Biomed Pharmacother, 2021, 133: 111083.
doi: 10.1016/j.biopha.2020.111083 pmid: 33378979 |
| [1] | GONG Zhi-hong, GONG Hong-ka, XU Yun, LIU Jun-pu, TU Yong-hong, XIE Hui-qun. Retrospective analysis of paragonimiasis cases in Jiangxi Province from 2011 to 2020 [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2022, 40(2): 247-251. |
| [2] | ZHANG Juan, XIA Jing, ZHANG Hua-xun, ZHU Hong, WU Dong-ni, WAN Lun, CAO Mu-min. Surveillance on Paragonimus infection in Hubei Province from 2018 to 2020 [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2021, 39(5): 600-605. |
| [3] | MA Zhi-qiang, WANG Lin, LI Sheng-hao, XU Jing-jing, LI Cai-xin, LIU Yuan, ZHANG Yan-ling, SHU Qiu-hong, ZHUANG Shan-shan, HE Shu Mei-qi, WANG Wen-lin, WANG Wei-qun. Preliminary study on autophagy of lung tissue cells in rats infected with Paragonimus proliferus [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2021, 39(1): 35-42. |
| [4] | NI Qing-xiang1*,LIN Xiao-yao2,YAO Li-nong3,RUAN Wei3,BAO Chang-xian2,CHEN Yi1,PAN Qiong-jiao1. An Investigation on a Case of Family-clustered Paragonimiasis in Wenzhou City [J]. , 2016, 34(5): 17-448. |
| [5] | LI Qiang1,2,QIN Da-ming3 *. Application of CT and MRI in the Diagnosis of Paragonimiasis in Brain and Spinal Cord [J]. , 2015, 33(1): 15-18-20. |
| [6] | GUO Mei, WANG Wei, JIANG Jian-Yu. Retrospective Analysis of 39 Child Cases of Paragonimiasis [J]. , 2011, 29(4): 17-251-253. |
| [7] | WANGShu-mei;;YANGFei-fei;HUANGYu-xian*;SHIGuang-fen;WENGXin-hua. Clinical Analysis of 78 Cases of Parasitic Encephalopathy [J]. , 2009, 27(3): 13-248. |
| [8] | HUYun-yun;ZENGLi-li;WANGYing. A case of encephalic paragonimiasis [J]. , 2008, 26(5): 21-399. |
| [9] | WANGYue;SHIXiao-hua;GANXiao-xian. Dot Immuno-Gold Filtration Assay in the Diagnosis of Suspected Paragonimiasis and Evaluation of Chemotherapeutic Effect [J]. , 2007, 25(1): 15-68. |
| [10] | YANQu-ru;YANTao;ZHOUXian-min;LIYou-song;ZHUChun-chao;SHILin-bo;MAXi-mei;HUNing-yan. Epidemiological Survey on the Infection of Paragonimus westermani in Jiangxi Province [J]. , 2004, 22(4): 15-252. |
| [11] | HUPeng;LIUYuehan. A Clinical Trial of Triclabendazole in the Treatment of Human Paragonimiasis skrjabini [J]. , 2001, 19(5): 14-307. |
| [12] | CHANGZhen-shan;WUBuo;BlairD;ZHANGYong-nian;HULing;CHENShao-hong;CHENMing-gang;FENGZhen;GeorgeM.Davis. GENE SEQUENCING FOR IDENTIFICATION OF PARAGONIMUS EGGS FROM A HUMAN CASE [J]. , 2000, 18(4): 6-215. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||