
CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES ›› 2024, Vol. 42 ›› Issue (1): 17-26.doi: 10.12140/j.issn.1000-7423.2024.01.003
• ORIGINAL ARTICLES • Previous Articles Next Articles
WANG Yebin1( ), SHEN Xuhang2, DENG Guoqiang1, HU Saimin1, WANG Fei3, ZHANG Lingling4, SHEN Jilong5,*(
), SHEN Xuhang2, DENG Guoqiang1, HU Saimin1, WANG Fei3, ZHANG Lingling4, SHEN Jilong5,*( )
)
Received:2023-08-09
Revised:2023-10-31
Online:2024-02-28
Published:2024-03-12
Contact:
*E-mail: Supported by:CLC Number:
WANG Yebin, SHEN Xuhang, DENG Guoqiang, HU Saimin, WANG Fei, ZHANG Lingling, SHEN Jilong. Effects of asymptomatic hookworm infection on intestinal microflora and metabolome in middle-aged and elderly people in rural area of Huangshan City[J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2024, 42(1): 17-26.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.jsczz.cn/EN/10.12140/j.issn.1000-7423.2024.01.003
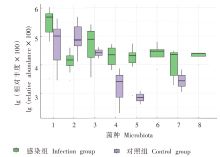
Fig. 3
Boxplot analysis of the top 8 of differential abundances of the intestinal microflora in the middle-aged and elderly people infected with hookworms in rural areas of Huangshan City 1: Prevotella; 2: B. vulgatus; 3: F. prausnitzii; 4: K. variicolla; 5: Parasutterrella; 6: Coprococus; 7: Clostridium UCG-014; 8: Enterobacterium.
Table 1
Indicator analyses of intestinal microflora in the feces of the middle-aged and elderly people infected with hookworms in rural areas of Huangshan City
| 序列号 Sequence ID | 菌门·属 Bacteria·Genus | 指示值 Indicator | |
|---|---|---|---|
| 感染组 Infection group | 对照组 Control group | ||
| ASV_195 | 厚壁菌门·真杆菌 Firmicutes·Eubacterium | 0.532 | 0.030 |
| ASV_121 | 拟杆菌门·另枝菌 Bacteroidota·Alistipes | 0.000 | 0.545 |
| ASV_174 | 拟杆菌门·拟杆菌 Bacteroidota·Bacteroides | 0.719 | 0.001 |
| ASV_318 | 脱硫杆菌门·嗜胆菌 Desulfobacterota·Bilophila | 0.051 | 0.516 |
| ASV_191 | 厚壁菌门·布劳特菌 Firmicutes·Blautia | 0.050 | 0.626 |
| ASV_206 | 变形菌门·Clade_Ⅰa Proteobacteria·Clade_Ⅰa | 0.000 | 0.727 |
| ASV_308 | 变形菌门·Clade_Ⅲ Proteobacteria·Clade_Ⅲ | 0.000 | 0.727 |
| ASV_105 | 厚壁菌门·梭菌UCG-014 Firmicutes·Clostridium_UCG-014 | 0.597 | 0.011 |
| ASV_87 | 厚壁菌门·粪球菌 Firmicutes·Coprococcus | 0.636 | 0.000 |
| ASV_28 | 厚壁菌门·小杆菌 Firmicutes·Dialister | 0.727 | 0.000 |
| ASV_165 | 变形菌门·肠杆菌 Proteobacteria·Enterobacterium | 0.727 | 0.000 |
| ASV_50 | 厚壁菌门·粪杆菌 Firmicutes·Faecalibacterium | 0.501 | 0.007 |
| ASV_523 | 变形菌门·HIMB1 Proteobacteria·HIMB11 | 0.000 | 0.454 |
| ASV_8 | 变形菌门·克雷伯菌 Proteobacteria·Klebsiella | 0.807 | 0.004 |
| ASV_284 | 厚壁菌门·Lachnoclostridium Firmicutes·Lachnoclostridium | 0.000 | 0.545 |
| ASV_584 | 拟杆菌门·Muribaculaceae Bacteroidota·Muribaculaceae | 0.010 | 0.403 |
| ASV_1 | 拟杆菌门·普雷沃菌 Bacteroidota·Prevotella | 0.833 | 0.106 |
| ASV_202 | 厚壁菌门·罗氏菌 Firmicutes·Roseburia | 0.455 | 0.000 |
| ASV_577 | 厚壁菌门·苏黎世杆菌 Firmicutes·Turicibacter | 0.012 | 0.474 |
| ASV_68 | 厚壁菌门·UCG-002 Firmicutes·UCG-002 | 0.520 | 0.009 |
| ASV_204 | 厚壁菌门·UCG-003 Firmicutes·UCG-003 | 0.028 | 0.571 |
| ASV_302 | 厚壁菌门·未鉴定属 Firmicutes·unclassified_genus | 0.422 | 0.006 |
| ASV_137 | 变形菌门·未鉴定属 Proteobacteria·Unclassified_genus | 0.531 | 0.002 |
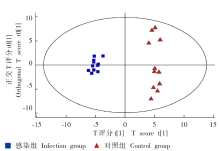
Fig. 4
OPLS-DA analysis of the metabolites in the fecal samples in the middle-aged and elderly people infected with hookworms in rural areas of Huangshan City R2X[1] = 0.113,R2Xo[1] = 0.080. The values of R2X[1] and R2X0[1] represent the interpretability of the predicted and orthogonal components on the dataset, respectively. Ellipse representation 95% CI of Hotelling T2 test.
Fig. 6
Enrichment analysis of differential metabolic pathways in the feces of the middle-aged and elderly people infected with hookworms in rural areas of Huangshan City 1: Protein digestion and absorption; 2: Central carbon metabolism in cancer; 3: Mineral absorption; 4: Aminoacyl-tRNA biosynthesis; 5: Neuroactive ligend-receptor interaction; 6: Pentose and glucuronate interconversion; 7: D-amino acid metabolism; 8: Arginine and proline metabolism; 9: Arginine biosynthesis; 10: Tyrosine metabolism; 11: Lysine degradation; 12: GABA ergic synapse; 13: Alarnine, aspartate and glutamate metabolism; 14: Synaptic vesicle cycle; 15: Glyoxylate and dicarboxylate metabolism; 16: Regulation of lipolysis in adipocytes; 17: ABC transporters; 18: Citrate cycle (TCA cyle); 19: Glycine, serine and threonine metabolism; 20: Phenylalanine metabolism.
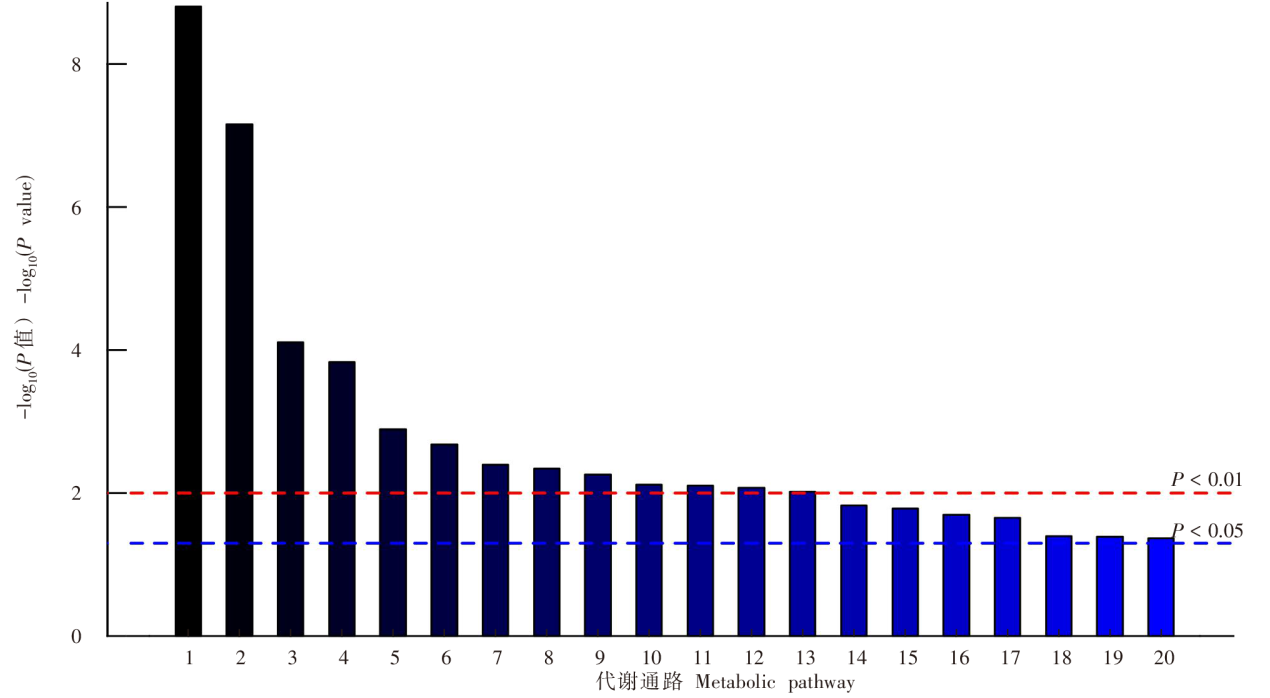

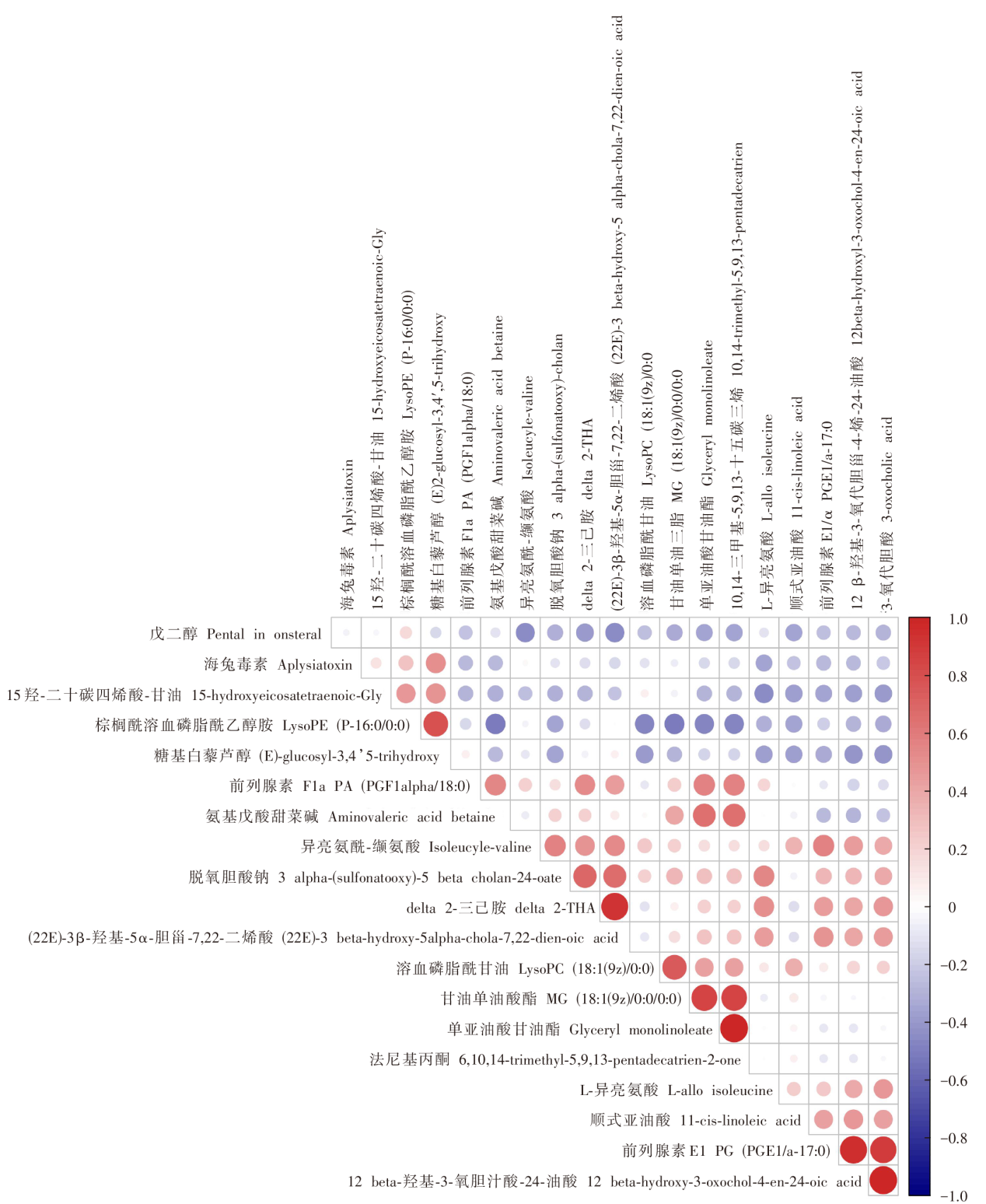
Fig. 7
Pearson’s correlation analysis of metabolomic differences in fecal specimens of the middle-aged and elderly people infected with hookworms in rural areas of Huangshan City Note: Red bubble indicates a positive correlation, while blue bubble indicates a negative correlation; the size of bubble indicates the size of the correlation coefficient.
| [1] | Zhang Y, Zhang SQ. Gut microbiome and health[M]. Beijing: China Light Industry Press, 2021: 1. (in Chinese) |
| (张彦, 张双庆. 肠道微生物组与健康[M]. 北京: 中国轻工业出版社, 2021: 1.) | |
| [2] |
Ni J, Wu GD, Albenberg L, et al. Gut microbiota and IBD: causation or correlation?[J]. Nat Rev Gastroenterol Hepatol, 2017, 14(10): 573-584.
doi: 10.1038/nrgastro.2017.88 pmid: 28743984 |
| [3] |
Singer-Englar T, Barlow G, Mathur R. Obesity, diabetes, and the gut microbiome: an updated review[J]. Expert Rev Gastroenterol Hepatol, 2019, 13(1): 3-15.
doi: 10.1080/17474124.2019.1543023 |
| [4] |
Christovich A, Luo XM. Gut microbiota, leaky gut, and autoimmune diseases[J]. Front Immunol, 2022, 13: 946248.
doi: 10.3389/fimmu.2022.946248 |
| [5] |
Witkowski M, Weeks TL, Hazen SL. Gut microbiota and cardiovascular disease[J]. Circ Res, 2020, 127(4): 553-570.
doi: 10.1161/CIRCRESAHA.120.316242 pmid: 32762536 |
| [6] |
Park EM, Chelvanambi M, Bhutiani N, et al. Targeting the gut and tumor microbiota in cancer[J]. Nat Med, 2022, 28(4): 690-703.
doi: 10.1038/s41591-022-01779-2 pmid: 35440726 |
| [7] |
Sampson TR, Debelius JW, Thron T, et al. Gut microbiota regulate motor deficits and neuroinflammation in a model of Parkinson’s disease[J]. Cell, 2016, 167(6): 1469-1480.e12.
doi: 10.1016/j.cell.2016.11.018 |
| [8] |
Nikolova VL, Smith MRB, Hall LJ, et al. Perturbations in gut microbiota composition in psychiatric disorders: a review and meta-analysis[J]. JAMA Psychiatry, 2021, 78(12): 1343-1354.
doi: 10.1001/jamapsychiatry.2021.2573 pmid: 34524405 |
| [9] |
Ling ZX, Liu X, Cheng YW, et al. Gut microbiota and aging[J]. Crit Rev Food Sci Nutr, 2022, 62(13): 3509-3534.
doi: 10.1080/10408398.2020.1867054 |
| [10] |
Parker A, Romano S, Ansorge R, et al. Fecal microbiota transfer between young and aged mice reverses hallmarks of the aging gut, eye, and brain[J]. Microbiome, 2022, 10(1): 68.
doi: 10.1186/s40168-022-01243-w pmid: 35501923 |
| [11] |
Coman V, Vodnar DC. Gut microbiota and old age: modulating factors and interventions for healthy longevity[J]. Exp Gerontol, 2020, 141: 111095.
doi: 10.1016/j.exger.2020.111095 |
| [12] | Zeng T, Lü S, Tian LG, et al. Temporal trends in disease burden of major human parasitic diseases in China from 1990 to 2019[J]. Chin J Schisto Control, 2023, 35(1): 7-14, 37. (in Chinese) |
| (曾婷, 吕山, 田利光, 等. 1990—2019年我国主要人体寄生虫病疾病负担变化趋势研究[J]. 中国血吸虫病防治杂志, 2023, 35(1): 7-14.) | |
| [13] |
Motran CC, Silvane L, Chiapello LS, et al. Helminth infections: recognition and modulation of the immune response by innate immune cells[J]. Front Immunol, 2018, 9: 664.
doi: 10.3389/fimmu.2018.00664 pmid: 29670630 |
| [14] |
Llinás-Caballero K, Caraballo L. Helminths and bacterial microbiota: the interactions of two of humans’ “old friends”[J]. Int J Mol Sci, 2022, 23(21): 13358.
doi: 10.3390/ijms232113358 |
| [15] |
Lund ME, Greer J, Dixit A, et al. A parasite-derived 68-mer peptide ameliorates autoimmune disease in murine models of type 1 diabetes and multiple sclerosis[J]. Sci Rep, 2016, 6: 37789.
doi: 10.1038/srep37789 pmid: 27883079 |
| [16] |
Cantacessi C, Giacomin P, Croese J, et al. Impact of experimental hookworm infection on the human gut microbiota[J]. J Infect Dis, 2014, 210(9): 1431-1434.
doi: 10.1093/infdis/jiu256 pmid: 24795483 |
| [17] | Mangiola F, Nicoletti A, Gasbarrini A, et al. Gut microbiota and aging[J]. Eur Rev Med Pharmacol Sci, 2018, 22(21): 7404-7413. |
| [18] |
O’Toole PW, Jeffery IB. Gut microbiota and aging[J]. Science, 2015, 350(6265): 1214-1215.
doi: 10.1126/science.aac8469 pmid: 26785481 |
| [19] |
Kim S, Jazwinski SM. The gut microbiota and healthy aging: amini-review[J]. Gerontology, 2018, 64(6): 513-520.
doi: 10.1159/000490615 |
| [20] |
Bravo JA, Forsythe P, Chew MV, et al. Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve[J]. Proc Natl Acad Sci USA, 2011, 108(38): 16050-16055.
doi: 10.1073/pnas.1102999108 |
| [21] |
Kim CS, Cha LN, Sim M, et al. Probiotic supplementation improves cognitive function and mood with changes in gut microbiota in community-dwelling older adults: a randomized, double-blind, placebo-controlled, multicenter trial[J]. J Gerontol A Biol Sci Med Sci, 2021, 76(1): 32-40.
doi: 10.1093/gerona/glaa090 |
| [22] |
Webster HC, Gamino V, Andrusaite AT, et al. Tissue-based IL-10 signalling in helminth infection limits IFNγ expression and promotes the intestinal Th2 response[J]. Mucosal Immunol, 2022, 15(6): 1257-1269.
doi: 10.1038/s41385-022-00513-y pmid: 35428872 |
| [23] | Hu ZH, Zhang CL, Sifuentes-Dominguez L, et al. Small proline-rich protein 2A is a gut bactericidal protein deployed during helminth infection[J]. Science, 2021, 374(6568): eabe6723. |
| [24] |
Su CW, Chen CY, Jiao LF, et al. Helminth-induced and Th2-dependent alterations of the gut microbiota attenuate obesity caused by high-fat diet[J]. Cell Mol Gastroenterol Hepatol, 2020, 10(4): 763-778.
doi: S2352-345X(20)30105-3 pmid: 32629118 |
| [25] |
Shimokawa C, Kato T, Takeuchi T, et al. CD8+ regulatory T cells are critical in prevention of autoimmune-mediated diabetes[J]. Nat Commun, 2020, 11(1): 1922.
doi: 10.1038/s41467-020-15857-x pmid: 32321922 |
| [26] | Franco-Lopez J, Duplessis M, Bui A, et al. Correlations between the composition of the bovine microbiota and vitamin B12 abundance[J]. mSystems, 2020, 5(2): e00107-e00120. |
| [27] |
Sokol H, Pigneur B, Watterlot L, et al. Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn disease patients[J]. Proc Natl Acad Sci USA, 2008, 105(43): 16731-16736.
doi: 10.1073/pnas.0804812105 |
| [28] |
Bush JR, Alfa MJ. Increasing levels of Parasutterella in the gut microbiome correlate with improving low-density lipoprotein levels in healthy adults consuming resistant potato starch during a randomised trial[J]. BMC Nutr, 2020, 6(1): 72.
doi: 10.1186/s40795-020-00398-9 |
| [29] |
Chen YJ, Wu H, Wu SD, et al. Parasutterella, in association with irritable bowel syndrome and intestinal chronic inflammation[J]. J Gastroenterol Hepatol, 2018, 33(11): 1844-1852.
doi: 10.1111/jgh.2018.33.issue-11 |
| [30] |
Rodríguez-Medina N, Barrios-Camacho H, Duran-Bedolla J, et al. Klebsiella variicola: an emerging pathogen in humans[J]. Emerg Microbes Infect, 2019, 8(1): 973-988.
doi: 10.1080/22221751.2019.1634981 |
| [31] | Zafar H, Saier MH Jr. Gut Bacteroides species in health and disease[J]. Gut Microbes, 2021, 13(1): 1-20. |
| [32] |
Iglesias-Vázquez L, van Ginkel Riba G, Arija V, et al. Composition of gut microbiota in children with autism spectrum disorder: a systematic review and meta-analysis[J]. Nutrients, 2020, 12(3): 792.
doi: 10.3390/nu12030792 |
| [33] |
Sakamoto M, Ikeyama N, Toyoda A, et al. Dialister hominis sp. nov., isolated from human faeces[J]. Int J Syst Evol Microbiol, 2020, 70(1): 589-595.
doi: 10.1099/ijsem.0.003797 |
| [34] |
Kong QM, Wang BT, Tian PJ, et al. Daily intake of Lactobacillus alleviates autistic-like behaviors by ameliorating the 5-hydroxytryptamine metabolic disorder in VPA-treated rats during weaning and sexual maturation[J]. Food Funct, 2021, 12(6): 2591-2604.
doi: 10.1039/D0FO02375B |
| [35] |
Chang TT, Chen JW. Direct CCL4 inhibition modulates gut microbiota, reduces circulating trimethylamine N-oxide, and improves glucose and lipid metabolism in high-fat-diet-induced diabetes mellitus[J]. J Inflamm Res, 2021, 14: 6237-6250.
doi: 10.2147/JIR.S343491 |
| [36] |
Liang JQ, Li T, Nakatsu G, et al. A novel faecal Lachnoclostridium marker for the non-invasive diagnosis of colorectal adenoma and cancer[J]. Gut, 2020, 69(7): 1248-1257.
doi: 10.1136/gutjnl-2019-318532 |
| [37] |
Loukas A, Hotez PJ, Diemert D, et al. Hookworm infection[J]. Nat Rev Dis Primers, 2016, 2: 16088.
doi: 10.1038/nrdp.2016.88 pmid: 27929101 |
| [38] | Gazzinelli-Guimaraes PH, Nutman TB. Helminth parasites and immune regulation[J]. F1000Res, 2018, 7: F1000FacultyRev-F1000Faculty1685. |
| [39] |
Loukas A, Maizels RM, Hotez PJ. The Yin and Yang of human soil-transmitted helminth infections[J]. Int J Parasitol, 2021, 51(13/14): 1243-1253.
doi: 10.1016/j.ijpara.2021.11.001 |
| [1] | LI Chang, DU Xinyue, YAN Min, WANG Zhaojun. Research advances on the role and mechanism of neutrophil extracellular traps in parasitic infection [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2023, 41(2): 219-222. |
| [2] | ZHONG Qiu-ting, SONG Jian-ping, LV Fang-li. The interactions between malaria and gut microbiota [J]. CHINESE JOURNAL OF PARASITOLOGY AND PARASITIC DISEASES, 2021, 39(4): 520-525. |
| [3] | LIU Jian-zhi,XIA Chen-yang*,FENG Jing,SONG Tian-zeng,MA Xing-bin,TANG Wen-qiang. Helminth Infections in Goats in Nimu County of Tibet [J]. , 2016, 34(1): 14-8-10. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||